

There are 2 pulses in the foot that to check for - the dorsalis pedis artery (DPA) and the posterior tibial artery (PTA). Palpating for pedal pulses is problematic. This clinical test, when positive, is a good predictor of a patient have PAD and CLI, but when negative, it does not mean there is not significant PAD or CLI.Ĭlinical findings of some value: Pulse palpation. When in a dependent position, the foot turns brightly red, called rubor, before returning to a normal pink color.
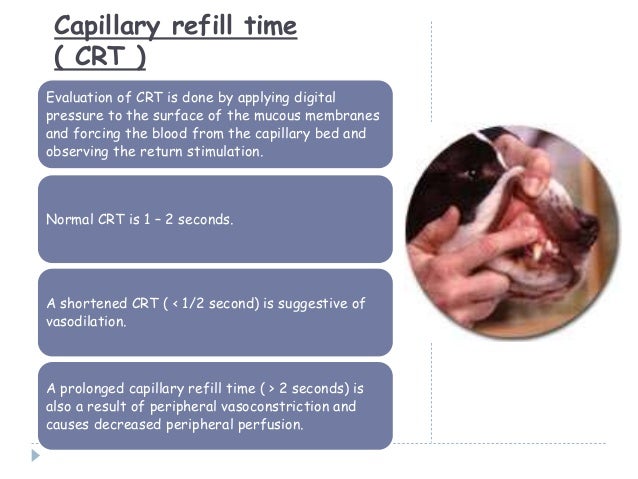
With elevation, the foot turns pale and there can be venous guttering (all the blood has drained out of the veins). In short, the negative predictive value of clinical findings for excluding clinically significant PAD is low.Ĭlinical findings of little value: Berger's Test (Examining the leg after elevation and then in a dependent position. However, if these findings are not present it does not mean that there is no PAD. Many of these findings, when present, are good predictors of PAD. Some of the common findings we look for are abnormal pulses, bruits (abnormal sounds from arteries), temperature differences, trophic changes (absent hair, thin dry skin, thickened nails), color changes and capillary refill. There are a variety of statistical terms we use to discuss the validity of these clinical findings such as sensitivity, specificity, negative predictive value, positive predictive value, true/false positive/negative and etc. When evaluating a patient for PAD we look for certain clinical findings to detect that the patient has or does not have the disease. Peripheral arterial disease (PAD) and its more severe variant critical limb ischemia (CLI) can be notoriously difficult to diagnose.


 0 kommentar(er)
0 kommentar(er)
